Why Do I Have IBS (10-15% of Population)? Causes and Solutions
You wake up with a knot in your stomach. The cramping starts before you get out of bed. You wonder if today will be another day of rushing to the bathroom or dealing with bloating.
Living with irritable bowel syndrome means your digestive system has its own schedule. The symptoms can make simple things like dinner or car rides stressful. You might plan bathroom stops or skip social events because of your body’s reactions.
Understanding your IBS is the first step to taking back control. While it affects up to 15% of Americans, everyone’s experience is different. Your journey with irritable bowel syndrome doesn’t have to limit your dreams.
Key Takeaways
- IBS affects 10-15% of the U.S. population, making it one of the most common digestive conditions
- Irritable bowel syndrome is a functional disorder that doesn’t damage your digestive tract or increase cancer risk
- Symptoms of IBS include abdominal pain, bloating, and changes in bowel habits
- Diagnosis relies on clinical criteria like Rome IV, as no single test can confirm IBS
- Multiple factors contribute to IBS, including diet, stress, and the gut-brain connection
- Treatment options range from dietary changes to medications and stress management techniques
Understanding IBS: Definitions and Symptoms
Living with digestive discomfort can be frustrating. You might not know what’s happening in your body. Irritable bowel syndrome (IBS) is a chronic condition that affects your digestive system. It doesn’t cause permanent damage to your intestines.
This functional disorder impacts how your gut works. It creates a pattern of symptoms that can significantly affect your daily life.
What is Irritable Bowel Syndrome?
IBS is a common digestive disorder that affects the large intestine. It’s different from inflammatory bowel diseases like Crohn’s disease or ulcerative colitis. IBS doesn’t cause inflammation or changes in bowel tissue.
Instead, it alters how your digestive system functions. This leads to uncomfortable symptoms that come and go over time.
Doctors classify IBS into four main types based on your primary symptoms:
- IBS-D: Primarily diarrhea
- IBS-C: Primarily constipation
- IBS-M: Mixed pattern of both
- IBS-U: Undefined subtype
Common Symptoms of IBS
The most common IBS symptoms include abdominal pain or cramping. This pain often improves after a bowel movement. You might also experience bloating, gas, and changes in bowel habits.
Some days you may have diarrhea, while other days bring constipation. Many people notice mucus in their stool or feel an urgent need to use the bathroom.
Beyond digestive issues, IBS can cause:
- Fatigue and sleep problems
- Anxiety or depression
- Headaches or migraines
- Chronic pelvic pain
How IBS Differs from Other Digestive Disorders
Understanding how IBS differs from other conditions helps you seek appropriate treatment. While IBS causes discomfort, it doesn’t damage your intestines or increase cancer risk. Blood in stool, weight loss, or fever aren’t typical IBS symptoms.
These signs might indicate inflammatory bowel disease or other serious conditions. Your doctor can determine the correct diagnosis through proper testing. They will evaluate your symptoms and medical history.
Prevalence of IBS in the United States
Looking into irritable bowel syndrome in America shows interesting facts. Millions of people in the U.S. live with this digestive issue every day. Studies have shown who gets IBS and when symptoms start.
Statistics on IBS Affected Individuals
About 10-15% of Americans have IBS symptoms. Women are twice as likely to have it, with 14% affected. Men have about 9%. Most symptoms start before people turn 40.
Only 30% of those with symptoms see a doctor for treatment for ibs. Many manage their symptoms on their own. IBS diagnosis goes down by 25% in people over 50. This could mean better management or changing symptoms with age.
Demographics: Who is Most Affected?
IBS doesn’t care about your income. It affects everyone, no matter their money situation. If you have a family history of IBS, your risk goes up. Many remember symptoms from childhood or young adulthood.
These irritable bowel syndrome statistics help doctors find and help at-risk groups. They can plan better care for these people.
Potential Causes of IBS
Learning what causes IBS can help you manage your symptoms. Scientists found that many factors contribute to this complex condition. Your digestive system links your gut and brain closely. When these connections break, IBS symptoms can start.
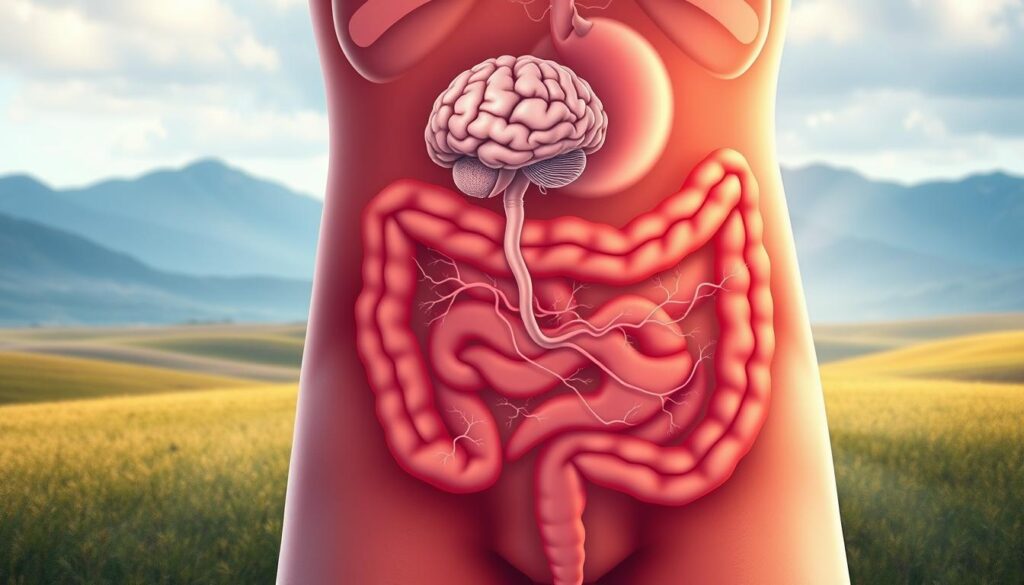
Gut-Brain Connection
Your gut has millions of nerve cells that talk to your brain. Recent studies show that ibs causes often come from hypersensitive nerves in your intestines. These nerves act differently than regular nerves. They can make you feel pain, bloating, or have irregular bowel movements.
Role of Diet and Lifestyle
What you eat and how you live affects your digestive health. Common ibs triggers include:
- Fatty or fried foods
- Dairy products
- Caffeine and alcohol
- Artificial sweeteners
- Large meals
Your daily habits also play a big role. Bad eating habits, not exercising, and poor sleep can make symptoms worse. Managing IBS often means finding your food triggers and sticking to routines.
Stress and Emotional Factors
Your feelings and stress levels affect your gut health. Many people see their symptoms get worse during stressful times. They get better when things calm down.
Stress hormones change how your gut moves and feels. Some people have random symptoms, while others have long periods of discomfort followed by calm times.
Diagnosis of IBS
Getting an accurate ibs diagnosis can feel like solving a puzzle without all the pieces. There’s no single test for irritable bowel syndrome. Doctors look at your symptoms and evaluate them carefully to see if you have IBS. Knowing the diagnostic process helps you get ready for your doctor’s visits.
Criteria for Diagnosis
Doctors use the Rome criteria to diagnose IBS. These criteria look at your symptom patterns over time. To get an ibs diagnosis, you must have abdominal pain at least three days a month for three months. This pain must also have two of these features:
- Pain improves after bowel movements
- Changes in how often you have bowel movements
- Changes in stool appearance or consistency
Importance of Medical Evaluation
A detailed irritable bowel syndrome evaluation helps rule out other conditions. Your doctor looks for signs that suggest other health issues. These include unexplained weight loss, blood in stool, severe nighttime symptoms, or symptoms starting after age 50. Early diagnosis means faster ibs relief through proper treatment.
| Evaluation Step | Purpose |
|---|---|
| Medical History | Identifies symptom patterns and duration |
| Physical Exam | Checks for abdominal tenderness or masses |
| Blood Tests | Rules out infections or inflammatory conditions |
| Stool Tests | Detects blood or parasites |
Dietary Modifications for IBS Sufferers
Your diet is key to managing IBS symptoms. What you eat affects how you feel every day. Finding the right ibs diet means knowing which foods are good for you and which cause problems. Everyone with IBS reacts differently to food, so making changes that fit you is important for treatment for ibs.
Low FODMAP Diet
The Low FODMAP diet is a top choice for managing ibs. FODMAPs are carbs that can upset some people’s stomachs. This diet has three steps: cutting out foods, trying them again, and finding what works for you.
| High FODMAP Foods | Low FODMAP Alternatives |
|---|---|
| Apples, pears | Strawberries, oranges |
| Wheat bread | Sourdough bread |
| Garlic, onions | Chives, garlic-infused oil |
| Milk, yogurt | Lactose-free milk, almond milk |

Importance of Fiber
Fiber is important in your ibs diet. Soluble fiber helps with bowel movements. Foods like oats and carrots can help. But, some people may find whole grains and raw veggies hard to digest. Start with small amounts and see how your body reacts.
Foods to Avoid
Some foods can upset people with IBS. These include:
- Carbonated drinks and alcohol
- Caffeine and chocolate
- Fried and fatty foods
- Artificial sweeteners like sorbitol
- Beans and cruciferous veggies
Keeping a food diary helps find out what bothers you. It’s a big help for treatment for ibs.
Lifestyle Changes to Manage IBS
Making the right lifestyle changes can really help your digestive health. Simple habits can make a big difference. By managing stress, staying active, and getting enough sleep, you can control your symptoms.
Stress Management Techniques
Stress can make your gut worse, leading to cramps and bloating. Managing ibs means learning to handle stress better.
- Practice deep breathing exercises for 5-10 minutes daily
- Try progressive muscle relaxation before bed
- Consider meditation apps like Calm or Headspace
- Join support groups to share experiences
Exercise and Its Benefits
Exercise is good for your digestion and can reduce IBS symptoms. It helps food move and releases happy hormones. Start slow and get more active as you feel better.
Walking, swimming, and yoga are great for IBS relief. Try to move for 30 minutes most days, but rest when you need to.
Sleep and Its Impact on IBS
Poor sleep can mess with your gut and make symptoms worse. Your digestive system needs rest to work right. Good sleep habits are key to managing IBS. Go to bed at the same time, avoid big meals before bed, and keep your room cool and dark.
Medications for IBS Relief
When diet and lifestyle changes aren’t enough, ibs medications can help. Finding the right treatment for ibs is a process. Your doctor will help create a plan based on your symptoms and needs.
Over-the-Counter Options
At your local pharmacy, you can find many ibs relief options. Antidiarrheals like loperamide (Imodium) help with loose stools. Fiber supplements, such as psyllium (Metamucil), help with bowel movements.
For gas and bloating, simethicone (Gas-X) breaks down gas bubbles. Peppermint oil capsules can reduce abdominal pain and cramping. Many also find relief with probiotics, which support healthy gut bacteria.
Peppermint oil capsules have shown promise in reducing abdominal pain and cramping. Many people also find relief with probiotics, which support healthy gut bacteria balance.
Prescription Medications
Your doctor may prescribe specific ibs medications based on your symptoms. For IBS with diarrhea, alosetron (Lotronex) or eluxadoline (Viberzi) can slow intestinal movement. If constipation is your main issue, lubiprostone (Amitiza) or linaclotide (Linzess) increase fluid in your intestines.
Antispasmodics reduce painful cramping. Low-dose antidepressants can help manage pain and bowel symptoms by affecting nerve signals between your gut and brain.
When to Consult a Doctor
Seek medical attention if symptoms interfere with daily activities. Look out for warning signs like unexplained weight loss, blood in stool, or severe abdominal pain. Your healthcare provider can rule out other conditions and develop an effective treatment for ibs tailored to your needs.
Alternative Therapies for IBS
When traditional treatments don’t work, many people try alternative IBS treatments. These natural methods help manage symptoms and improve life quality. Everyone is different, so it may take some time to find what works best.
Acupuncture and Its Benefits
Acupuncture is a promising way to manage IBS symptoms. It involves thin needles in specific body points to balance energy. Studies show it can lessen pain, bloating, and bowel issues.
Many patients feel more relaxed and have better digestion after acupuncture.
Probiotics and Gut Health
Your gut has trillions of bacteria that impact digestion and health. Probiotics add good bacteria to balance your gut. For IBS, *Bifidobacterium infantis* and *Lactobacillus plantarum* are best.
You can find probiotics in yogurt, kefir, and supplements. Start with small amounts to let your body adjust.
Herbal Remedies
Many herbs can help with IBS symptoms. Peppermint oil capsules relax intestinal muscles, reducing pain. Ginger helps with nausea and bloating.
Chamomile tea soothes inflammation. Fennel seeds aid digestion and reduce gas. Always talk to your doctor before trying herbal remedies, as they can interact with medicines.
Coping Strategies for Living with IBS
Living with IBS can feel very isolating. Symptoms can really disrupt your daily life. It’s important to find ways to cope.
Building connections, educating others, and tracking your symptoms can help. This way, you can take control of your condition. It can also improve your quality of life.
Building a Support Network
Having a strong support system is key for managing IBS. Start by connecting with:
- Local IBS support groups where you can share experiences
- Online communities through forums like IBS Network or Reddit’s r/ibs
- Family members and close friends who understand your condition
- Mental health professionals specializing in chronic conditions
Remember, you’re not alone. About 10-15% of Americans have IBS symptoms. Finding others who get it can make living with IBS easier.
Educating Others About IBS
It’s important to clear up misconceptions about IBS. This can help reduce stigma and improve your relationships. When explaining your condition, focus on:
- Describing IBS as a real medical condition affecting the gut-brain connection
- Explaining how symptoms can vary from day to day
- Setting boundaries about what accommodations you need
- Sharing resources from organizations like the International Foundation for Gastrointestinal Disorders
Journaling and Tracking Symptoms
Keeping a symptom diary is a powerful tool for managing IBS. Most people have symptoms on more than half their days. Tracking helps spot patterns. Record:
- Daily food intake and meal times
- Stress levels and emotional state
- Sleep quality and duration
- Symptom severity and duration
- Bathroom habits and consistency
Use apps like Cara Care or MySymptoms to make tracking easier. This data is very helpful when working with healthcare providers. It helps them create personalized IBS support strategies.
The Role of Healthcare Professionals
Managing IBS needs ibs healthcare from skilled doctors. Your journey starts with finding a gastroenterologist who knows IBS well. They use detailed checks and known methods to make plans just for you.
Finding the Right Healthcare Provider
Choosing the right gastroenterologist is key for treatment for ibs. Look for doctors who focus on digestive issues and have IBS experience. The Cleveland Clinic suggests picking doctors who look for IBS first, not other conditions.
- Board certification in gastroenterology
- Experience treating IBS patients
- Communication style that makes you comfortable
- Availability for follow-up appointments
- Willingness to explore various treatment options
Importance of Ongoing Support
Regular medical support is key to managing IBS. Your team should keep an eye on you and change treatments when needed. Guidelines say that managing IBS well needs a long-term partnership with your doctor.
| Support Type | Frequency | Benefits |
|---|---|---|
| Regular Check-ups | Every 3-6 months | Monitor symptom changes |
| Treatment Adjustments | As needed | Optimize symptom relief |
| Emergency Consultations | When symptoms worsen | Prevent complications |
Future Outlook for IBS Research
IBS research is moving fast as scientists learn more about it. They’ve found out about gut nerve sensitivity and how your gut and brain talk to each other. These new findings are leading to new treatments that could change how doctors help people with IBS in the future.
Advances in IBS Treatments
Teams at places like Mayo Clinic and Johns Hopkins are making new medicines. These medicines might help with nerve sensitivity or fix gut-brain communication. Right now, clinical trials are testing new drugs that target the real causes of IBS, not just the symptoms.
Importance of Continued Research
More research on IBS is key because some IBS patients might get inflammatory bowel disease soon. Studies show IBD is much more common in people with IBS symptoms. This shows why we need better ways to tell IBS apart from inflammatory diseases.
Potential Breakthroughs on the Horizon
The next ten years could bring big changes in IBS treatment. Scientists at Stanford and UCLA are working on blood tests to find out what kind of IBS someone has. This could lead to treatments that really work for people with IBS.